How Does Diabetes Cause Necrosis?
Necrosis, defined as the premature and irreversible death of tissue, is a severe complication frequently associated with long-standing diabetes mellitus. While multiple organ systems can be affected by hyperglycemia-induced damage, the lower extremities—particularly the feet—are at disproportionate risk due to microvascular impairment and peripheral neuropathy. Diabetic necrosis is not merely a cosmetic or localized concern; it represents a critical point in disease progression that often precedes infection, gangrene, and ultimately, amputation. Recognizing the underlying mechanisms that lead to necrosis is essential for clinicians and patients alike to implement preventive strategies and reduce morbidity.
What Is Necrosis?
Necrosis refers to the pathological process by which cells and tissues undergo irreversible death due to external injury, ischemia, infection, or metabolic derangement. Unlike apoptosis, which is a programmed and orderly form of cell death, necrosis is uncontrolled and often triggers inflammatory responses that further compromise surrounding tissue. In the context of diabetes, necrosis is most commonly precipitated by sustained hyperglycemia that impairs oxygen delivery and nutrient perfusion, ultimately leading to cellular breakdown. Histologically, necrotic tissue appears eosinophilic, structureless, and may exhibit calcification or bacterial colonization in advanced cases. Clinically, cutaneous necrosis manifests as areas of skin discoloration, ulceration, or eschar formation, particularly in pressure-prone or poorly perfused regions.
How Diabetes Leads to Necrosis
The pathogenesis of necrosis in diabetic patients is multifactorial, primarily driven by chronic hyperglycemia and its systemic vascular and neurological sequelae. Persistent elevated blood glucose levels induce endothelial dysfunction, promoting atherosclerosis and compromising microcirculatory flow. Concurrently, diabetic peripheral neuropathy diminishes protective sensation, allowing minor injuries—such as abrasions, blisters, or pressure ulcers—to go unnoticed and untreated. The resultant ischemia and unrelieved trauma create a hypoxic environment conducive to tissue breakdown. Furthermore, impaired leukocyte function in diabetes hampers host defense, increasing susceptibility to infection, which accelerates necrotic progression. Collectively, these factors establish a cascade of cellular hypoxia, immune failure, and tissue degradation that underpins diabetic necrosis, particularly in the lower limbs.
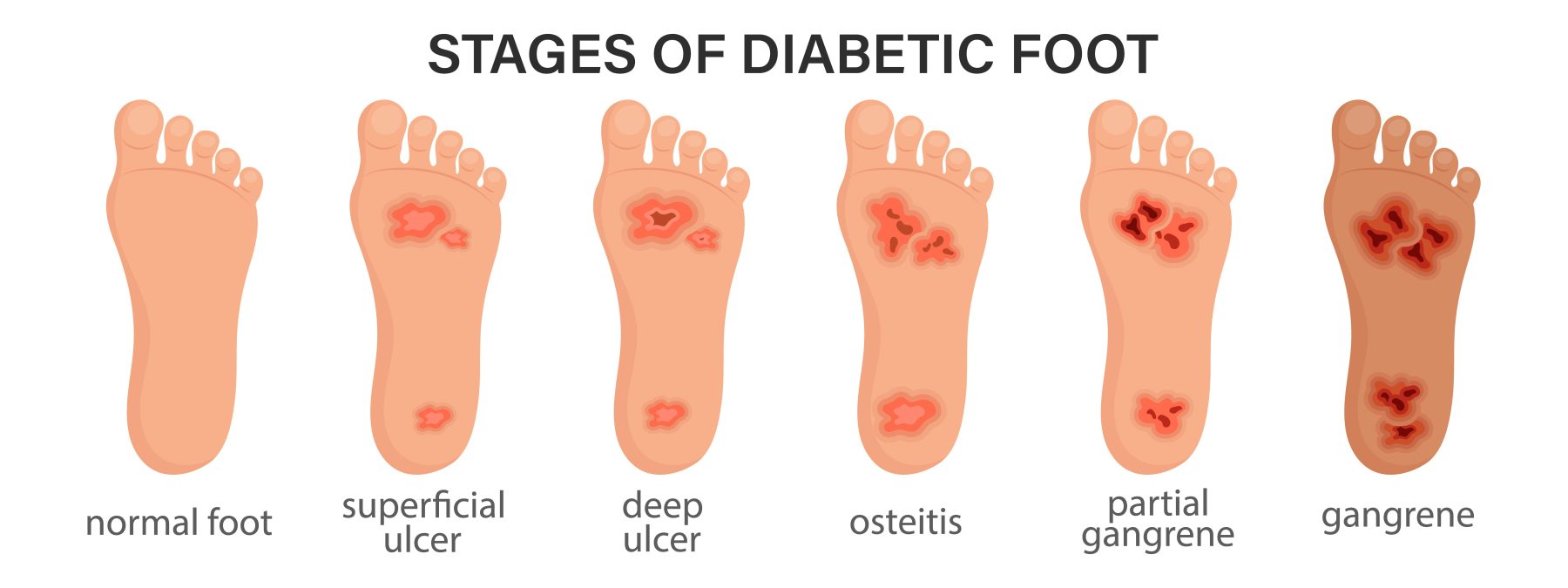
Stages of Risk: Diabetic Foot Grading
To assess the risk of necrosis and other complications, clinicians utilize diabetic foot grading systems that stratify patients based on sensory, vascular, and structural abnormalities. This approach enables timely intervention and tailored surveillance. The following are standard clinical grades:
- Grade 0: No neuropathy; intact protective sensation. Minimal risk, but ongoing screening is essential.
- Grade 1: Sensory neuropathy present without foot deformity. Diminished sensation increases the risk of unnoticed injury.
- Grade 2: Neuropathy combined with peripheral arterial disease (PAD) and/or structural deformities (e.g., claw toes, Charcot foot). Pressure redistribution is impaired, increasing the risk of skin breakdown.
- Grade 3: History of foot ulceration, infection, or amputation. This group has the highest risk of recurrence, necrosis, and limb loss.
As patients advance through these grades, the likelihood of ischemic injury, poor wound healing, and subsequent tissue necrosis rises exponentially, underscoring the need for early risk identification and proactive care.
How to Prevent Diabetic Necrosis
Preventing necrosis in patients with diabetes requires a multidisciplinary strategy centered on metabolic control, routine foot care, and early detection of pre-ulcerative changes. Glycemic management remains the cornerstone; maintaining HbA1c within individualized target ranges reduces microvascular and neuropathic progression. Daily foot inspections are essential, with patients advised to examine for fissures, erythema, calluses, or temperature asymmetry using mirrors or caregiver assistance. Proper hygiene, including gentle washing with pH-balanced soap and thorough drying—especially between toes—minimizes fungal and bacterial colonization. Clinicians should recommend therapeutic footwear with pressure-relieving insoles to prevent repetitive trauma. Additional preventive measures include:
- Smoking cessation to improve peripheral perfusion.
- Weight optimization to reduce plantar pressure.
- Routine podiatric evaluations, particularly in high-risk individuals.
- Immediate medical attention for any signs of skin breakdown or infection.
Preventive adherence significantly lowers the incidence of necrosis and its associated morbidities.
How Feetsee Helps Detect Problems Before It’s Too Late
Feetsee is an FDA-registered, contact-free thermal imaging device engineered for daily at-home monitoring of diabetic foot health. By capturing over 19,000 thermal data points per foot, it detects subtle temperature variations indicative of early inflammation—often before visual signs appear. The device integrates with a mobile app, sending real-time alerts and sharing data with healthcare providers to support timely intervention. Its design requires no standing or contact, making it ideal for patients with limited mobility or sensory loss.
Take Control of Your Foot Health Today
Necrosis is a preventable consequence of poorly managed diabetes, but prevention requires vigilance and the right tools. Feetsee empowers patients with evidence-based, real-time monitoring that bridges the gap between routine care and daily risk. By integrating technology into your foot care regimen, you gain an early warning system against inflammation, ulcers, and eventual tissue death. For individuals living with diabetes, proactive detection isn’t optional—it’s lifesaving. Choose Feetsee and take the first step toward long-term limb preservation.
References:
https://www.jwmr.org/upload/pdf/jwmr-2023-02747.pdf
https://www.sciencedirect.com/science/article/abs/pii/S0895796719300110
https://link.springer.com/chapter/10.1007/978-3-031-60954-1_53

Detect Early, Prevent Amputations
Diabetic foot ulcers (DFUs) lead to significant discomfort, pain, numerous amputations, and billions of dollars in healthcare costs each year.
