What is Diabetic Neuropathy — Symptoms and Treatment
Diabetic neuropathy is a progressive complication of chronic hyperglycemia, characterized by nerve fiber injury that predominantly affects the peripheral nervous system. It results from sustained metabolic and microvascular dysfunction caused by elevated blood glucose levels, ultimately impairing nerve conduction and structure. Clinically, it presents as a spectrum of sensorimotor and autonomic disturbances, with symptoms ranging from distal paresthesia and numbness to gastrointestinal dysmotility and orthostatic hypotension. Diabetic neuropathy not only diminishes quality of life but also increases the risk of foot ulceration, infection, and limb amputation, making early identification and intervention critical in diabetic care.
Types of Diabetic Neuropathy
Diabetic neuropathy can be classified into four primary types, each affecting distinct areas of the nervous system, with varying clinical manifestations.
Peripheral Neuropathy
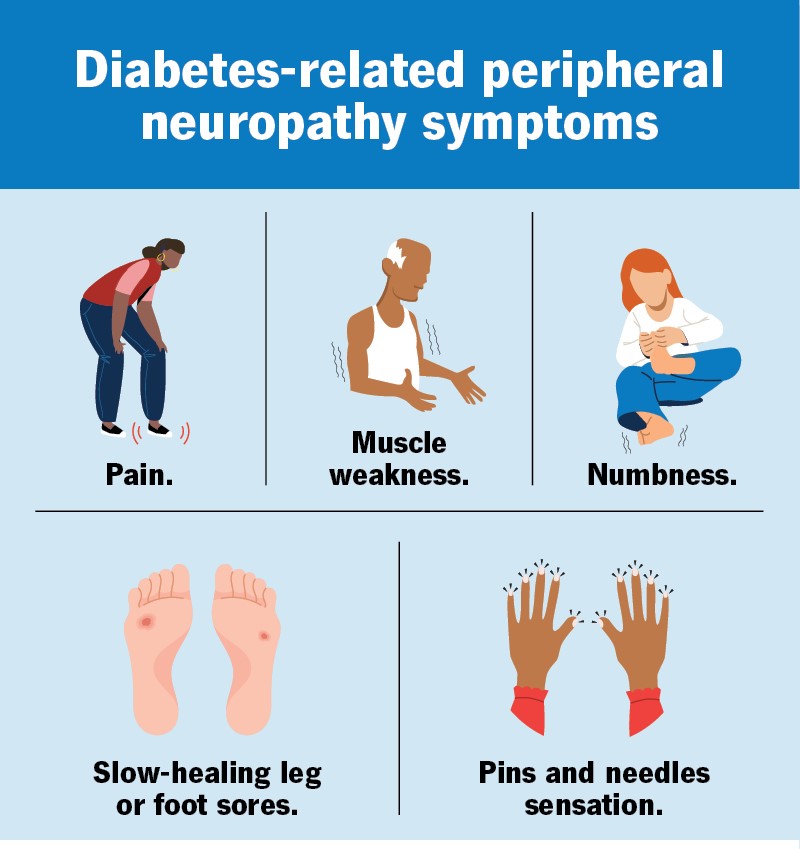
Peripheral neuropathy is the most common type of diabetic neuropathy, primarily affecting the feet, legs, and sometimes the hands and arms. This condition arises due to nerve damage caused by prolonged high blood sugar, which disrupts the sensory fibers responsible for transmitting sensations from the extremities. Symptoms can range from numbness and tingling to more severe pain, often worsening at night. Without proper management, this form of neuropathy can lead to significant loss of sensation, increasing the risk of unnoticed injuries or foot ulcers.
Autonomic Neuropathy
Autonomic neuropathy results from damage to the autonomic nervous system, which regulates involuntary bodily functions. This type of neuropathy can affect the heart, gastrointestinal tract, urinary system, and sexual organs, leading to a wide variety of symptoms. Common issues include orthostatic hypotension (a sudden drop in blood pressure when standing), gastroparesis (delayed stomach emptying), urinary retention, and sexual dysfunction. In some cases, autonomic neuropathy can also cause hypoglycemia unawareness, making it difficult to recognize low blood sugar levels, which poses a significant safety risk.
Proximal Neuropathy
Proximal neuropathy affects the nerve roots in the thighs, hips, and buttocks. It often presents as sudden, severe pain in one side of the body, particularly in the lower extremities. This form of neuropathy may also result in muscle weakness, difficulty rising from a sitting position, and, in more severe cases, muscle atrophy. Unlike peripheral neuropathy, proximal neuropathy tends to affect larger nerve areas and can be disabling if not appropriately managed.
Mononeuropathy (Focal Neuropathy)
Mononeuropathy, also referred to as focal neuropathy, involves damage to a single nerve, which may occur in the face, torso, or limbs. This localized nerve damage can lead to sudden and severe symptoms, including double vision, facial paralysis, or weakness in the hand, which may result in difficulty gripping objects. While focal neuropathy can be distressing, it is often temporary and may improve over time with proper treatment.\
Causes and Risk Factors
Causes of Diabetic Neuropathy
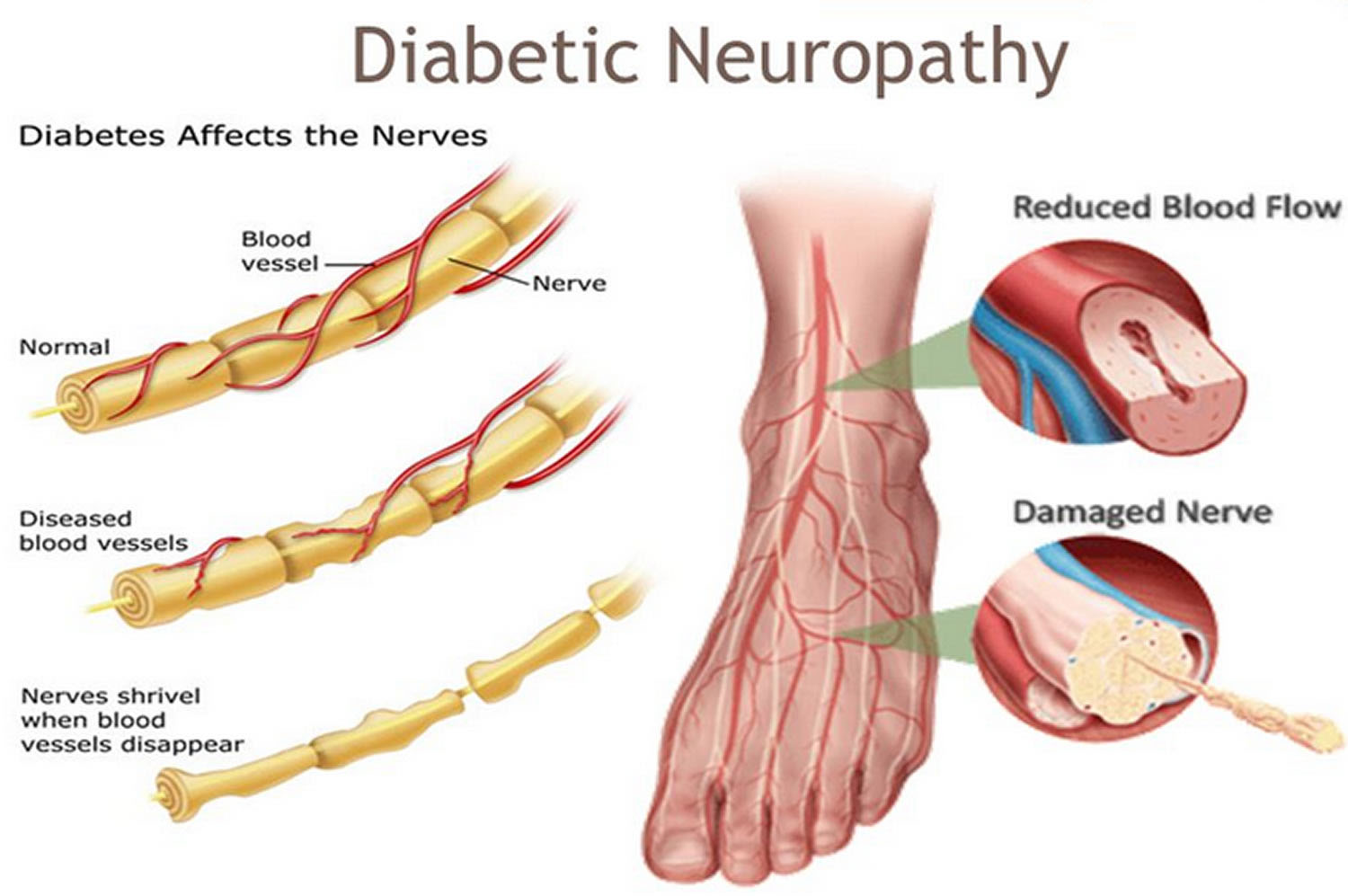
The primary cause of diabetic neuropathy is prolonged hyperglycemia, which damages the small blood vessels supplying oxygen and nutrients to the nerves. Over time, this insufficient blood flow leads to nerve fiber injury and impaired nerve function. Chronic high blood sugar levels trigger a cascade of metabolic changes, including oxidative stress, inflammation, and glycation of proteins, all of which contribute to nerve damage. Additionally, metabolic factors like increased blood pressure and elevated cholesterol levels may exacerbate the condition by further compromising nerve health.
Risk Factors for Diabetic Neuropathy
Several factors increase the likelihood of developing diabetic neuropathy in individuals with diabetes. The most significant risk factor is the duration of diabetes—those with a longer history of diabetes are at higher risk. Poor glycemic control also plays a critical role; patients with an A1C level above 7% are at a substantially increased risk of neuropathy. Other risk factors include high blood pressure, obesity, high cholesterol, kidney disease, smoking, and alcohol use disorder. Additionally, there is growing evidence suggesting that genetic predisposition may also influence susceptibility to neuropathic complications in diabetes.
Diagnosing Diabetic Neuropathy
Diagnosing diabetic neuropathy begins with a comprehensive medical history and an assessment of the patient’s glycemic control. Healthcare providers typically inquire about symptoms such as numbness, pain, and tingling in the extremities, as well as issues related to autonomic function. The physical exam often includes a detailed neurological assessment, focusing on the sensory function in the feet and hands. Routine tests include monofilament testing to check for pressure sensitivity, and vibration tests using a tuning fork to assess nerve conduction.
For a more definitive diagnosis, additional electrophysiological tests such as nerve conduction studies (NCS) and electromyography (EMG) may be employed to measure the speed and efficiency of electrical signals traveling through the nerves. In cases where autonomic neuropathy is suspected, heart rate variability testing or gastric emptying studies may be utilized to assess autonomic function. Early screening for neuropathy is essential, especially in individuals with long-standing diabetes, as early detection enables better management and prevents further progression.
Treatment for Diabetic Neuropathy
The primary goal of treating diabetic neuropathy is to manage symptoms, prevent progression, and address the underlying cause: chronic hyperglycemia. Tight glycemic control is paramount, as maintaining an A1C level below 7% has been shown to reduce the incidence and severity of neuropathy. Pharmacological management focuses on alleviating pain and discomfort associated with neuropathy. Commonly prescribed medications include gabapentin, pregabalin, and duloxetine, all of which target nerve pain through various mechanisms, such as inhibiting neurotransmitter release and stabilizing nerve activity.
For individuals with autonomic neuropathy, treatment is tailored based on the specific system affected. Beta-blockers may be used to manage tachycardia or high heart rate, while prokinetic agents like metoclopramide are often employed to treat gastroparesis. Physical therapy is beneficial for those experiencing muscle weakness or impaired mobility, particularly in peripheral and proximal neuropathy. Occupational therapy and speech therapy may also be required for individuals with hand or swallowing difficulties, respectively.
For more advanced cases or when conservative measures fail, surgical interventions such as nerve decompression may be considered in cases of focal neuropathy. Acupuncture and alternative therapies may also provide symptom relief, although evidence for their effectiveness remains mixed. Ultimately, managing diabetic neuropathy requires a multidisciplinary approach involving endocrinologists, neurologists, and pain management specialists to optimize care and improve quality of life.
Can Diabetic Neuropathy Be Reversed?
Unfortunately, diabetic neuropathy is generally considered irreversible once nerve damage has occurred. However, early intervention and effective glycemic control can significantly halt or slow the progression of the condition. In the initial stages of neuropathy, where nerve function may still be intact, symptom management through proper blood sugar regulation can lead to significant improvement in sensory symptoms such as pain and tingling. Additionally, pharmacological therapies aimed at reducing nerve inflammation and oxidative stress have shown some promise in improving nerve function, particularly when treatment is initiated early.
As the damage progresses, especially in more advanced cases, the potential for complete reversal of neuropathic changes diminishes. In these instances, treatment shifts from reverse to symptom control and prevention of complications, such as ulcers or amputations. Regular monitoring and timely intervention are critical in maintaining quality of life for those affected by severe neuropathy. While nerve regeneration is unlikely, pain management and preserving mobility can still significantly improve patient outcomes.
Living with Diabetic Neuropathy
Living with diabetic neuropathy presents ongoing challenges, as the condition often causes chronic pain, muscle weakness, and loss of sensation in the affected areas. These symptoms can impair an individual’s ability to perform daily tasks, making it essential to adopt strategies for managing both physical and emotional aspects of the condition. Foot care is particularly important, as numbness and poor circulation can increase the risk of unnoticed injuries and infections. Regular self-exams and professional foot checks are critical in preventing ulcers or wounds from developing into serious complications.
In addition to physical management, individuals living with neuropathy often face emotional and psychological challenges, including depression and anxiety related to the loss of independence and quality of life. Psychosocial support, through therapy or support groups, plays a vital role in helping individuals cope with the emotional burden of living with a chronic condition. Moreover, adaptations such as mobility aids, orthotic footwear, and home modifications (e.g., removing tripping hazards) can improve safety and reduce the risk of falls.
With proper medical care, lifestyle adjustments, and ongoing support, individuals with diabetic neuropathy can continue to lead active lives. However, it is crucial to stay engaged with healthcare providers for routine monitoring and to adjust the treatment plan as necessary to address new or worsening symptoms.
Why Early Monitoring Matters — Try Feetsee
Early detection of diabetic neuropathy is essential for preventing severe complications such as foot ulcers, infections, and amputations. Unfortunately, neuropathy often develops silently, with many individuals experiencing little to no symptoms in the early stages. This makes proactive monitoring crucial. Feetsee offers an innovative, FDA-registered solution to help individuals manage their foot health before visible symptoms appear. By using thermal imaging technology, Feetsee detects subtle changes in foot temperature that often precede nerve damage, allowing for early intervention.
Unlike traditional methods, Feetsee’s non-invasive, contactless monitoring system provides an easy-to-use tool for daily at-home monitoring, helping you stay ahead of potential issues. The data gathered is automatically shared with your healthcare provider, ensuring collaboration and timely action. This proactive approach can significantly reduce the risks of severe complications, including the need for costly interventions or amputation.
By incorporating Feetsee into your routine, you take control of your foot health, ensuring that you catch issues early and prevent long-term damage. Don’t wait for symptoms to worsen—with Feetsee, you can stay ahead of diabetic neuropathy and maintain your independence with confidence.
References:
https://diabetesjournals.org/compendia/article/2022/1/1/147001/Diagnosis-and-Treatment-of-Painful-Diabetic
https://www.sciencedirect.com/science/article/pii/B9780128206690000141
https://www.sciencedirect.com/science/article/pii/S2666396120300078

Detect Early, Prevent Amputations
Diabetic foot ulcers (DFUs) lead to significant discomfort, pain, numerous amputations, and billions of dollars in healthcare costs each year.
